Historical Steps in Establishing Diagnostic Criteria for Grading Stenosis of Brain Supplying Arteries: A Litmus Test for Clinical Usefulness
Article information
Abstract
This publication describes the development of the diagnosis of stenosing diseases of brain-supplying arteries using ultrasound Doppler sonography, based on the personal experience of the author. It starts with the search test of flow alteration at the ophthalmic arteries as evidence of upstream obstruction and ends with the examination of extra- and intracranial arteries using Color Duplex technology. The advantage of ultrasound diagnostics is the good morphological description of the wall changes together with the assessment of hemodynamics. A meaningful assessment of the degree of stenosis requires knowledge of existing collateral circulation. The clinical utility of this method is in constant flux, depending on new therapeutic methods.
INTRODUCTION
The author has been involved in the development of neurovascular ultrasound since 1974. This publication presents some aspects illustrating the role of ultrasound in grading stenosis or occlusion of arteries supplying blood to the brain. The emphasis is on the clinical usefulness of this method. Is Doppler ultrasound a low-cost screening method that is fast and easy to perform, or a reliable method for grading disease and adding hemodynamic information and helpful in making clinical decisions?
The clinical value of any diagnostic method is unstable because it depends on multiple constantly changing factors.
1) Cost and possible harm in comparison to other available methods
2) Availability and standardization
3) Reliability for clinical decisions
4) New or evolving treatment options
It is interesting to see from where we have come to appreciate the present technology. However, less attention is presently given to earlier techniques and criteria to help solve diagnostic problems.
It must be remembered that previous information about the technical and diagnostic progress in different areas of the world was hardly available, and dissemination was relatively slow. Therefore, this presentation is subjective and incomplete. The development of available techniques in different periods will be demonstrated, focusing on arteriosclerotic disease in the extracranial arteries of the brain. This has been a prevalent problem in western countries and has influenced the development of clinical applications. In Japan, Doppler sonography was invented and established by Satomura and Kaneko.1 Their research was oriented to vascular physiology rather than arteriosclerotic disease of extracranial arteries, which was less prevalent in Japan. Therefore, this part of history is not the subject of this study.
CONTINUOUS-WAVE DOPPLER (CW DOPPLER)
The first technique for the clinical application of vascular ultrasound to detect carotid artery occlusion was continuous-wave Doppler (CW Doppler) sonography. Doppler shift signals are detected using a handheld pencil probe. There is no information about the depth of recording or the angle of insonation. Therefore, the signal analysis is mainly based on the audio signal of the Doppler frequencies. Documentation was made possible with a zero-crossing meter, allowing the registration of an analogous waveform, but not the Doppler shift or the spectrum of frequencies quantitatively.
1. Examination technique
Clinicians were accustomed to examining the arteries of the legs by pulse palpation. Similarly, the branches of the ophthalmic artery were the first to be examined to detect obstructions of the internal carotid artery (ICA) using the Doppler ophthalmic test.2,3 This was analogous to the ophthalmodynamometry used to detect ICA occlusion by reduced intraocular pressure. The Doppler ophthalmic test recorded the direction of flow using compression tests (compression of the superficial temporal and facial arteries) (Fig. 1). Reverse flow was reduced after compression, indicating occlusion or significant carotid artery stenosis. The initial expectation that differences in the amplitude of the signal of the supratrochlear artery, a branch of the ophthalmic artery, would indicate stenosis was not confirmed. However, zero flow or reversed flow is a sign of severe stenosis or occlusion without differentiating between them. Currently, direct visualization of the carotid arteries with Duplex sonography is highly sensitive to any degree of vessel narrowing. Nevertheless, the finding of a reverse flow with the Doppler ophthalmic test is still a valuable criterion for hemodynamically relevant carotid obstruction. Despite being useful, fast, and easy to perform, this test is frequently omitted because appropriate devices and probes are not available.
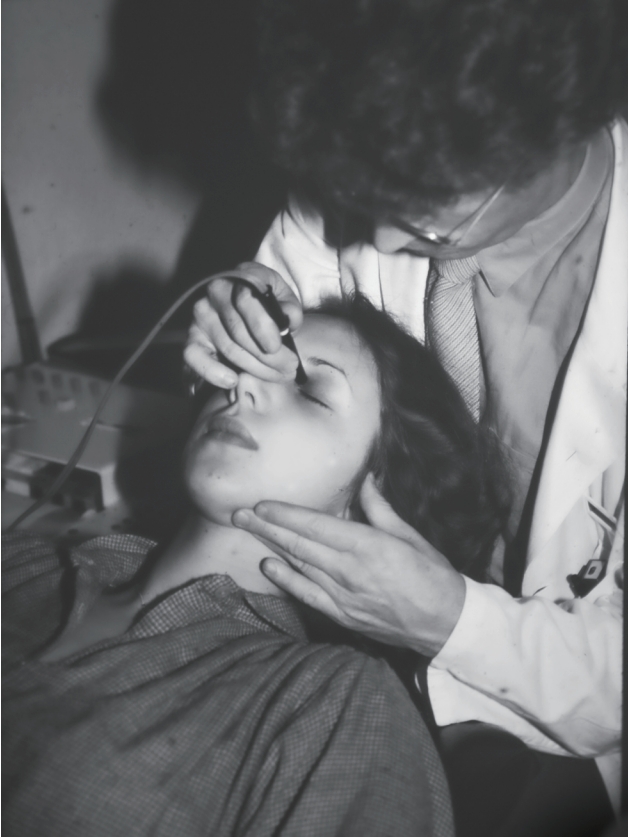
Doppler ophthalmic test. The examiner is sitting behind the patient. The probe is positioned on the supratrochlear artery, a branch of the ophthalmic artery. Simultaneous compression of the superficial temporal and facial arteries can be seen. In case the flow is reduced or reversed during compression, the flow in the ophthalmic artery is reversed, which is a sign of internal carotid artery obstruction.
Recording the common carotid artery (CCA) waveforms was an early part of the test, as it was easily detectable.3 The aim was to detect side-to-side differences in signal amplitude. A higher pulsatility was observed in cases of distal obstruction. This was added to the Doppler ophthalmic test and was useful, especially in cases of ICA occlusion. Less significant side-to-side differences in the pulsatility of the CCA waveform can be detected in cases of significant ICA stenosis. An immediate comparison of both sides was required to determine the difference in the audio signal. In addition, the waveform and audio signal of the CCA differ considerably in the case of ICA occlusion, as opposed to occlusion of the external carotid artery (ECA). Awareness of this difference increases the diagnostic yield significantly, even when using modern Duplex technology.
The next step for CW Doppler sonography was direct insonation of the ICA and the external carotid artery (ECA) and its branches. Initially, this seemed impossible due to the multitude of vessels in the neck. However, in normally perfused arteries, the difference in pulsatility of the ICA compared to the ECA makes it easier to differentiate by continuously moving the probe from the CCA over the bifurcation (Fig. 2). In cases of ICA occlusion, it is not possible to detect a normal or stenotic signal in the ICA. Therefore, compression tests (compression or tapping of the superficial temporal, facial, occipital artery, or thyroid gland) were used to identify all ECA branches (Fig. 3).4,5 In cases of ICA occlusion, all the signals beyond the bifurcation can be identified as belonging to the ECA and its branches. This allowed a positive predictive value (PPV) for ICA occlusion of ≈90%. The PPV for high degree stenosis of the ICA was even higher despite a rather basic technology compared to the modern Color Duplex sonography. A basic grading of ICA obstructions was possible (Fig. 4). For the first time, the vertebral arteries were examined noninvasively.4,6
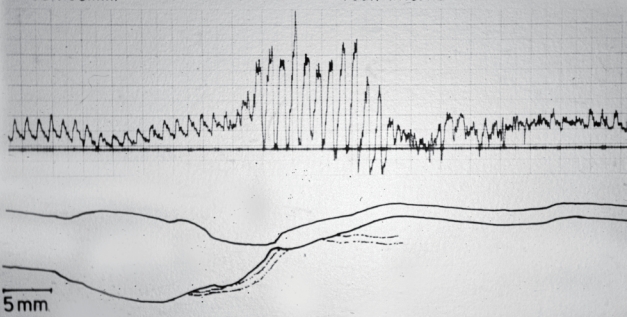
Continuous-wave Doppler examination of the carotid artery of a patient with high degree stenosis of the internal carotid artery (ICA). Continuous registration during movement of the probe from the common carotid artery (left side) to ICA. Slow flow indicates an enlarged bulb of the ICA. Sudden increase in frequency at the level of stenosis and post-stenotic disturbances are observed. Registration with a zero-crossing meter. The pathologic waveform at the stenosis (inverted systolic peaks) is due to a combined sample of high (stenosis) and low frequencies (post-stenotic eddies). The drawing below is from the angiogram.
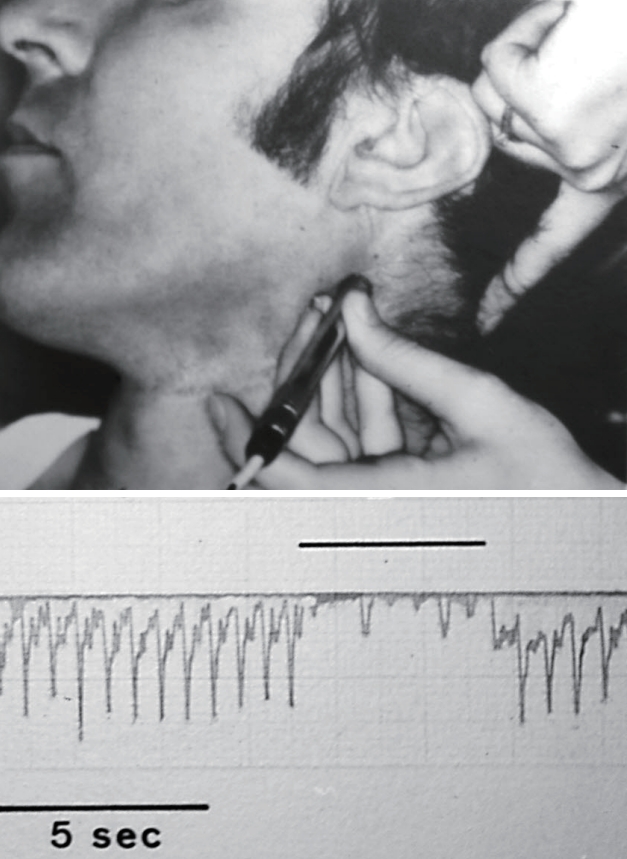
Identification of a branch of the external carotid artery (ECA). Distal compression of the occipital artery leads to cessation of flow in the proximal segment of this artery. Similarly, all branches of the ECA can be identified.
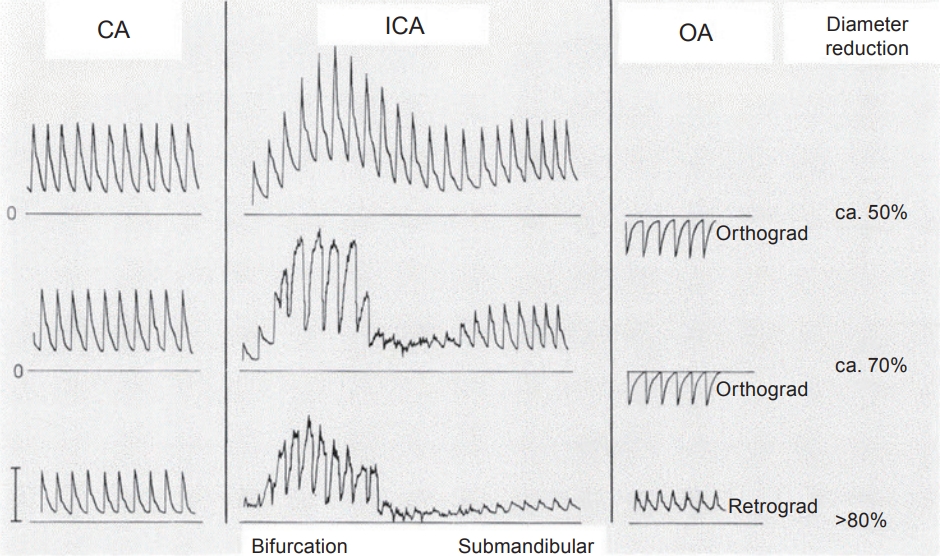
Grading carotid stenosis with continuous-wave Doppler sonography. Common carotid artery: diastolic flow velocity is reduced only in cases of very high-grade internal carotid artery (ICA) stenosis. ICA: with a 50% local diameter reduction, there is an increased flow velocity, but only a few post-stenotic disturbances. The audio signal of 70% stenosis is indicating high Doppler frequencies and more post-stenotic disturbances, but still a normalization of the submandibular flow. With >80% stenosis, reduced post-stenotic flow is observed. Ophthalmic artery: a reversal of flow direction is seen only in cases of high-degree stenosis (collateral flow). Modified from Büdingen et. al.4
2. Value of examining with a CW Doppler pencil probe
1) Fast examination of the branches of the ophthalmic artery
2) Free movement and angulation to obtain the best signal with the lowest insonation angle
3) The ease of following the course of a vessel, especially small vessels, such as the occipital artery
3. Position in the clinical setting
In the late 70s, the alternative diagnostic method was X-ray angiography, often performed by direct puncture of the CCA or retrograde brachial artery injection, both rather painful procedures, and therefore restricted to differential diagnosis and symptomatic patients. There was also a 1 to 2% incidence of causing a stroke. Sonography alone as the guiding method to indicate carotid surgery was an exception.7 This was true even when experienced sonographers were available. Carotid surgery was a frequent procedure without evidence from randomized controlled trials, which was the same for medical treatment. But on the other hand, the increased use of the non-invasive ultrasonic method provided better knowledge about the incidence, the pathophysiologic role, and prognosis of occlusive disease. For example, it became evident that the subclavian steal effect was asymptomatic in most patients.
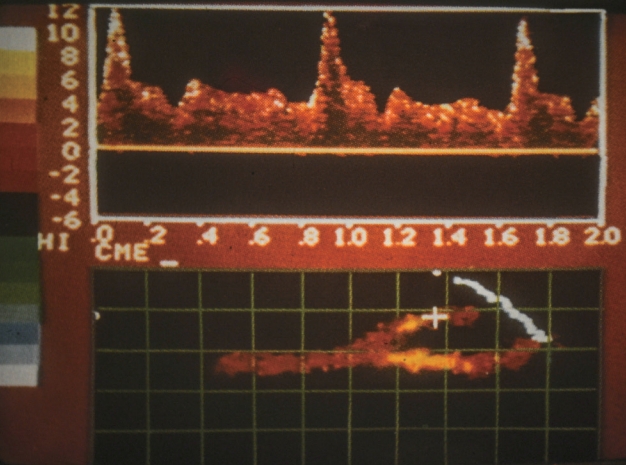
Flow imaging was used to improve the documentation of CW Doppler examination. The probe was passed back and forth across the neck and any Doppler signal was recorded on a computer screen (Fig. 5).8 The signal could be color-coded to demonstrate the frequency shift. The result was an approximate picture of the carotid artery, showing the presence of a greater than 60% stenosis. This technique could be performed by a technician after little training, and it provided an image that the referring physician could appreciate. Doppler flow imaging is mainly used in North America, where the test is performed by vascular technicians and not by a physician, unlike most European countries.
SPECTRUM ANALYSIS
CW Doppler, using a zero-crossing meter technique for registration, did not allow measuring the envelope of the spectral waveform. The peak systolic frequency (PSV) is today a popular criterion for determining the degree of stenosis. Only a rough estimate was possible listening to the audio signal. The next step forward was a quantitative waveform analysis. Today we know about the limited value of PSV taken as the predominant criterion for grading.9-11 Spectrum analysis does not add much to listening to the audio signal for grading. The same holds for the quantitative analysis of post-stenotic flow disturbances. It was hoped one would be able to detect minor disease by a quantitative analysis of the spectral broadening of Doppler frequencies due to disturbed flow after a wall irregularity, a plaque.
The audio signal contains this information and can be qualified as light, moderate, or severe by listening. Spectrum analysis can measure the disturbance of flow quantitatively by measuring the bandwidth of frequencies (-velocities). The bandwidth is narrow in the case of laminar flow and is wide with disturbances.12 The hope of detecting low degree stenosis by less pronounced post-stenotic disturbances was disappointed. These disturbances are seen as well after the bending in elongated vessels. Flow separation and a “disturbed velocity spectrum” are normal findings in the enlarged ICA bulb as it is at any branching. Listening to the audio signal is similarly sensitive for detecting abnormal flow. The detection and localization of increased wall thickness and plaques is today the field of modern B-Mode technology.
1. Added value of spectrum analysis
Spectrum analysis improves the documentation of the spectral waveform, including the PSV and identification of artifacts or abnormal flow, such as oscillating flow in cerebral circulatory arrest or alternating flow direction of the vertebral artery, which is observed with an incomplete subclavian steal effect.4,6 Spectrum analysis is beneficial for teaching.
2. Position in the clinical setting
CW Doppler sonography documented by spectrum analysis did not significantly improve the detection of high degree stenosis of the ICA. This value became more evident in Duplex sonography. On the other hand, spectrum analysis is essential for embolus detection and differentiation from artifacts.
COLOR DUPLEX SONOGRAPHY
Duplex sonography combined with B-Mode imaging and Doppler sonography is the current standard. The quality of the first available devices did not allow B-Mode imaging of fine structures. Imaging combined with the pulsed Doppler technique made it possible to determine the depth of recording, define the sample volume, and estimate the angle of insonation. The results could now be expressed as the velocity in cm/s instead of the Doppler frequency. The advantage is the independence of the velocity results from the emission frequency of the device. The disadvantages were the higher variability of measurements owing to different flow velocities, depending on the location of the sample on the flow profile over the vessel diameter. Another limitation is the problem of recording very high velocities with pulsed Doppler emission, limited by the Nyquist frequency (half of the emitted frequency). Owing to the width of the linear probe, it is more difficult to obtain a small angle of insonation compared to handling a pencil probe. The higher the angle of insonation, the higher is the possible error in the velocity estimate. The next step was color flow imaging.13 Flow toward the probe and away are represented in different colors and velocities in shades from dark to light. The color indicates the lumen of the artery and stenosis with a reduced diameter. However, owing to the slow frame rate, it is possible that the color is smeared over the border of the B-Mode image. On the other hand, shadowing or insufficient color flow visualization of the whole lumen due to low velocity is a limiting factor. Therefore, color cannot demonstrate the true vessel lumen of stenosis. It can be used to follow the vessel course and localize areas with increased velocities, indicating stenosis. In addition, color can demonstrate the direction of flow lines and is therefore helpful for the adjustment of the angle of insonation to convert frequencies into velocities. These flow lines could differ considerably from the orientation of the vessel axis (Fig. 6).
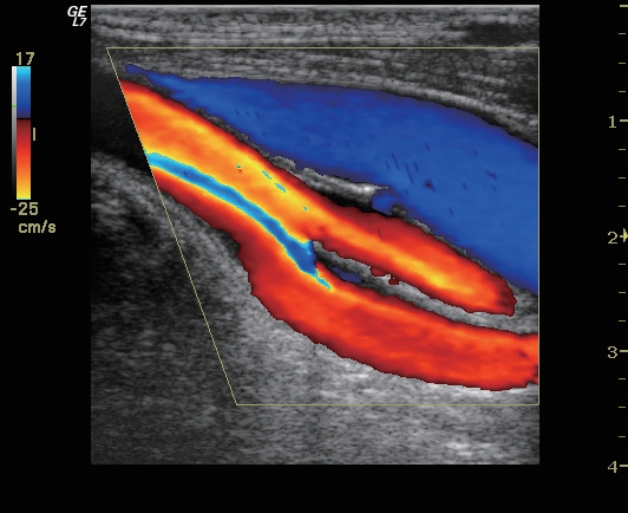
Color flow imaging and angle correction. Figure denotes carotid bifurcation, With common carotid artery on the left side. Imaging of flow lines indicated by shades from red to yellow or by aliasing will be helpful to determine the correct incidence angle for Doppler sonographic velocity estimation. The flow lines often deviate from the vessel axis.
1. Added value of color duplex sonography
With color duplex, all grades of carotid artery disease can be investigated, from increased intima-media thickness to nearly occluded arteries. This generates meaningful documentation. The full capability of duplex color flow imaging provides complex hemodynamic and morphological information. However, each function, B-Mode, pulsed Doppler, and color, require an individual manual adjustment and device setting to obtain all the information. This increases the complexity of the test and the need for training and teaching the technical background.
2. Position of the color duplex in the clinical setting
Color duplex of the carotid arteries helps guide clinical decisions in patients with a history of TIA or stroke. It is the first-line examination, together with brain imaging, for classifying an ischemic event in large artery disease, possible microvascular origin, or cardioembolism. Carotid artery duplex alone is insufficient. The posterior circulation must be examined, at least in the prevertebral and vertebral segments. The decision to operate on carotid stenosis should not be based solely on carotid duplex. Additional examinations of the intracranial collateral pathways are needed.
TRANSCRANIAL DOPPLER AND DUPLEX SONOGRAPHY
One of the first applications of ultrasound was the A-scan midline echography. This occurred in the 60s and 70s. It was a well-known routine examination together with electroencephalography (EEG) for all patients with focal symptoms because imaging of the brain with a computed tomography (CT) scan was not available. There was a general belief that the skull bone was a barrier for Doppler sonography with an emission frequency of 4 MHz. It was only in 1981 and 1982 that Aaslid, an engineer, and Nornes, a neurosurgeon, developed and published Transcranial Doppler sonography (TCD).14 They used a similar low emission frequency in use for a long time for A-scan midline echography and the first electronic sector scan developed for intracranial B-Mode imaging studies.15 Already with this sector scan, vascular pulsations could be registered. Therefore, it is remarkable that more than a decade passed before the introduction of TCD. Subsequently, transcranial color Doppler (TCCD) was performed using the same scan head as that used for transthoracic echocardiography. TCD opened new applications, such as follow-up of vasospasm, detection of intracranial stenosis, or documentation of cerebral circulatory arrest. In addition, the question of whether ICA stenosis is pressure-reducing and hemodynamically relevant can be based on the examination of the circle of Willis.
THE LAST CRITERION ADDED FOR GRADING: POSTSTENOTIC VELOCITY AND DIAMETER
Imaging of the post-stenotic distal segment of the ICA requires special handling. One needs to position the probe >2 cm distal to the origin of the enlarged bulb to reach the submandibular region, distal to possible post-stenotic flow disturbances. This is the region of reference for the NASCET criterion of stenosis. The examination of this segment is essential for two reasons, first the diagnosis of complete occlusion (imaging of the post-stenotic, occluded segment without flow) and second for differentiation of higher grades based on the reduced post-stenotic PSV: ≥50 cm (≈70% [NASCET]), <50 cm/s (≈80%), ≤30 cm/s (≈90%).9 Together with a reduced velocity, there is a reduction in the diameter of the distal ICA (≤3 mm). In X-ray angiography, this is known as a collapsed artery.16 The PSV can be lower despite more severe stenosis.9 A reduced post-stenotic PSV was the last, important criterion added to the German and WFN guidelines for grading. At the time of publication, it was based more on personal experience than comparative studies. A recent study supports low velocity and reduced vessel diameter as a criterion for grading within high degree stenoses (Fig. 7).17
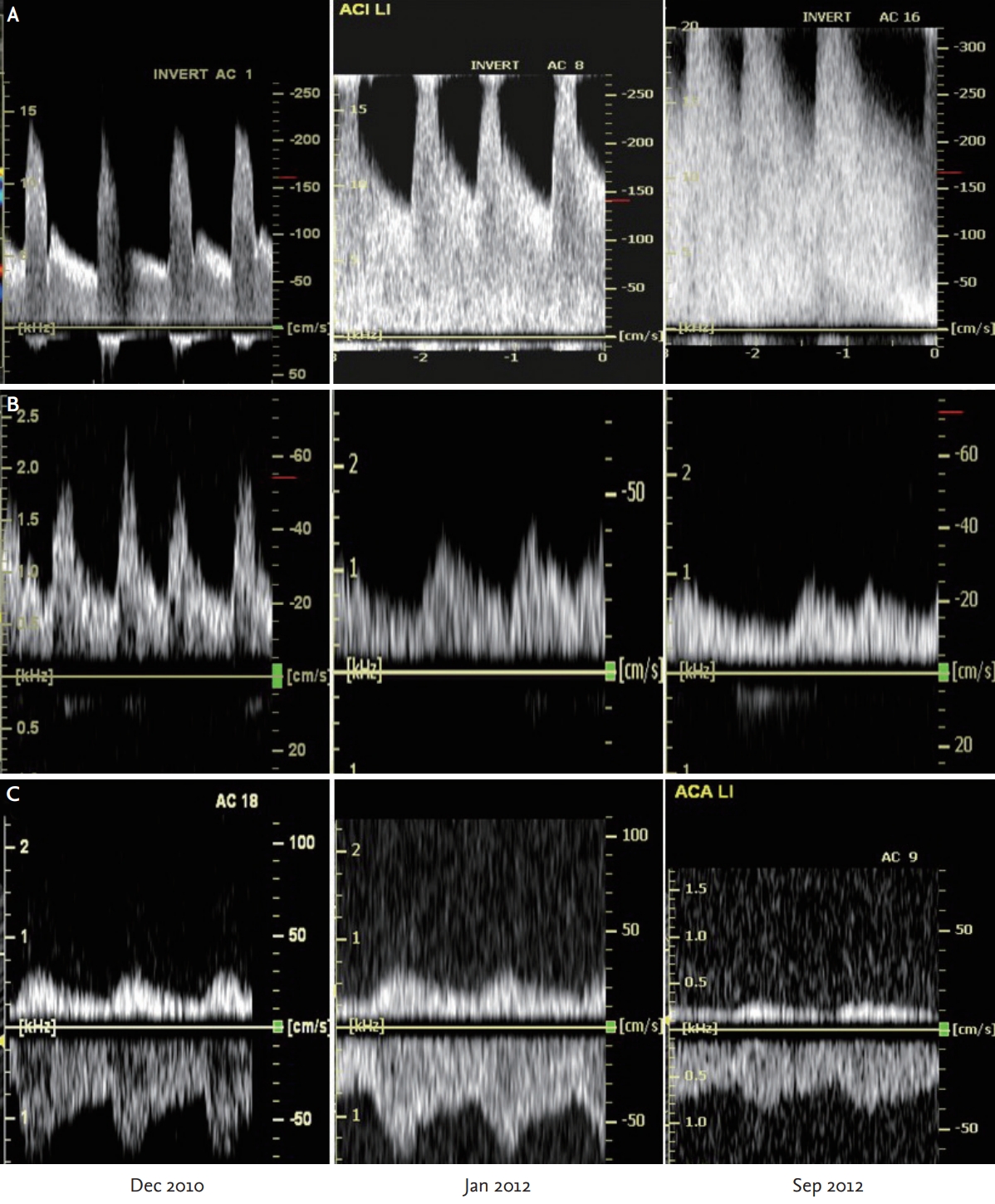
Follow-up of an asymptomatic patient presenting an increasing degree of stenosis. Recording of the distal internal carotid artery (ICA) and the intracranial arteries is helpful for grading. (A) Spectral waveform of the ICA stenosis. (B) Recording of the distal submandibular segment of the ICA. (C) Transcranial recording of the ipsilateral anterior cerebral artery (ACA) with flow direction away from the probe (below the zero line). Dec 2010: initial examination. Jan 2012: with increasing peak systolic velocity of the stenosis, the velocity of the distal ICA is lowered below 50 cm/s. Sep 2012: distal ICA <30 cm/s, indicating a ≈90% ICA stenosis. In the first study with normal waveform and flow direction of the ACA, but the progressing degree of stenosis, the systolic upstroke is less steep and the velocity and pulsatility are markedly reduced. The absence of crossflow (flow reversal) suggests an incomplete circle of Willis; either the right ACA or the anterior communicating artery is aplastic or hypoplastic. In the case of complete occlusion of the ICA, the patient would be at an increased risk of stroke because of inadequate collateral supply. Therefore, carotid artery surgery is recommended.
1. Position in the clinical setting
Using the TCD and TCCD, we evaluate the anterior and posterior cerebral arteries at the base of the skull and its main branches, including the basal circle of Willis. The ophthalmic artery as a collateral pathway, despite diagnostic interest, has little hemodynamic effect. The circle of Willis is often incomplete, or its branches are asymmetric in diameter. Therefore, collateral capacity is variable and significantly influences the PSV of pressure-reducing extracranial stenosis. This is the main reason for the large scatter of results comparing the PSV with the diameter of stenosis measured by arteriography.9 Therefore, combining extraand transcranial Ultrasound examination describes the hemodynamic effect of stenosis and allows meaningful grading. Selective bilateral digital subtraction angiography yields comparable information but is an invasive procedure that is seldom performed. CT and magnetic resonance (MR)-angiography cannot provide similar hemodynamic information. Decisions to operate or treat with stenting are based on complete ultrasonic and clinical data. The precondition is that the examination be fully documented and performed by a physician with level 3 experience (teaching level). Additionally, a final test should be performed shortly before any intervention. The same holds true for follow-up of asymptomatic patients. Extra-and transcranial examinations allow for deciding whether there is a transition from a moderate to a high degree of stenosis (Fig. 7). In acute stroke, Doppler ultrasound (TCD) was expected to be a useful initial test.18 There was hope for sonothrombolysis as a treatment of intracranial large artery occlusion. With the present move to thrombectomy, Doppler ultrasound should be the method for follow-up (recanalization, re-occlusion) because it is repeatable and can be performed at the bedside. On arrival at the emergency department, there is generally not enough time for additional vascular examinations besides CT or MR angiography.
DISCUSSION
At the beginning of the ultrasonic method, a clear separation was observed. Ultrasound Doppler provided hemodynamic information, and invasive angiography was mainly morphologic. CW Doppler was a screening method, and invasive radiologic angiography was limited to severely affected patients. The change occurred with improved B-Mode, color imaging, and noninvasive CT and MR technology. The progress in quality was parallel for all the ultrasonic and radiologic methods. Therefore, it is difficult and complicated to compare the relationships between these methods over time. This is the never-ending story; the same problem for all methods. Knowledge of the technical basics and handling skills (training) is required to obtain reliable information. The time for training in the learning phase is presently the limiting factor. This leads to specialization.
Imaging wall structures and the flow with color is eye-catching, attracting more attention than Doppler audio signals or subtle changes in the spectral waveform. We started with a pencil probe that we moved along an artery while listening to the audio Doppler signal and ended up in front of a complex cockpit (like riding a bicycle and finally driving a racing car).
When a method is in the development phase and opens new application areas, there is much drive to achieve excellent results. However, an annoying routine task lowers reliability. Therefore, there is a need for 3-level ultrasound diagnostic services for difficult examinations, clinical decisions, and unusual findings, such as preoperative evaluation, moyamoya disease, dissection, or inflammation.
The value of Doppler ultrasound for clinical decisions is highly dependent on the treatment options. Asymptomatic carotid stenosis can be treated with endarterectomy or stenting when progression to hemodynamically relevant stenosis is observed (Fig. 7). Follow-up with ultrasound Doppler is the best method for timely decision-making. Plaque morphology is another known prognostic factor. Of interest is not only the gray-scale analysis and surface of plaques, but also plaque perfusion,19 waiting for additional studies. The problem in generating evidence for all these questions is that a long observation period is needed to see endpoints or to collect a sufficiently large number of subjects in a randomized study.
FINAL COMMENT
There has been a continuous and partially unexpected stepwise development of the ultrasonic methods for grading disease of the arteries to the brain since the late 60s of the last century. It started as a screening method but has developed into the first-line examination or a complementary non-invasive method to other imaging modalities, such as CT or MR angiography, depending on the clinical situation and possible treatment options. Based on previous experience, expanded technical capabilities will also open up new, possibly unexpected, diagnostic possibilities for subsequent generations of neurological ultrasonographers. However, it is important to be able to perform these examinations and investigate the cause of any unusual findings.
Notes
Ethics statement
The Institutional Review Board process and patient consents were not proceeded because of a review article.
Availability of Data and Material
The data that support the findings of this article are available in the text.
Sources of Funding
None.
Conflicts of Interest
No potential conflicts of interest relevant to this article was reported.
Acknowledgements
I thank Al Persson M.D. for his review and helpful comments.