Pheochromocytoma-related Headache and Symptoms that Should Not be Overlooked: A Case Report
Article information
Abstract
When a patient complaining of headache comes to the hospital, the focus is usually on checking for neurological disorders. After these are excluded, functional headaches are usually thought of, and it is easy to overlook other causes. In the case presented here, a patient was hospitalized with a severe headache. There were no specific findings in either brain imaging or cerebrospinal fluid. The severe headache persisted, accompanied by excessive sweating. As the cause was unclear, chest and abdomen computed tomography was taken, where an adrenal gland mass was confirmed. With a diagnosis of pheochromocytoma, the patient improved with treatment. This triad of symptoms (headache, sweating, and palpitations) should raise suspicion of pheochromocytoma; however, most patients do not present with all three symptoms. Because of this, if headaches persist without other neurological symptoms, further evaluation should be performed to determine other possible causes such as pheochromocytoma.
There are over 200 types of headaches that have been identified to date, and many conditions can cause various headaches; some are not dangerous, but some are life-threatening. The headache description and specific neurological examination findings determine whether further examinations are needed and what management strategy is best. As a neurologist, when a patient comes to the hospital complaining of severe headache, examination is usually focused on looking for neurological disorders such as brain tumors, infections, or cerebrovascular disease. After the above are excluded, functional headaches are usually thought of next, including migraine, tension, or psychogenic headaches; this means it is easy to overlook other possible causes. A challenging case is presented here that should not be overlooked, where a patient presented to a neurology outpatient clinic complaining of severe headache.
CASE
A 53-year-old male was hospitalized with a severe headache. His symptoms began abruptly three days before presentation; pulsatile and crushing headache on the left side, at 8 or above on the numeric rating scale, a level that he had never felt before. The headache got worse when he moved and persisted even after taking painkillers, and was severe enough to wake him with excessive sweating. He was so nauseous that he couldn’t eat. The patient had no recent history of fever or upper respiratory or urinary tract infection and had not received any recent vaccinations. He also denied a previous history of illness. His only medical history was diabetes mellitus which was well-controlled with medication. He was a social drinker and current smoker who had been smoking for 30 years. He reported he had been under a lot of work stress as an automobile repair adviser. Neurological examination did not show any specific findings except for mild trapezius tenderness on the right side. When admitted to hospital, his temperature was 36.0°C, his blood pressure was 100/70 mmHg, his heart rate was 75 BPM, and his respiratory rate was 20 breaths/min. Serum electrolytes, glucose, C-reactive protein, free T4, and thyroid-stimulating hormone were normal, as well as liver and renal function tests, complete blood counts with differentials, and erythrocyte sedimentation rate.
To rule out secondary causes in the intracranial structure, brain magnetic resonance imaging (and magnetic resonance angiography were performed immediately after admission. There were no major abnormalities on either, except for a 2 cm lipoma on the left occipital scalp and focal high signal intensity lesion in periventricular white matter on fluid attenuated inversion revcovery (FLAIR) images (Fig. 1A-C). Magnetic resonance venography was performed subsequently to rule out cerebral venous sinus thrombosis (Fig. 1D). Overall, there were no specific findings. Cerebrospinal fluid was unremarkable for the presence of white or red blood cells, glucose, or protein. There were no specific findings from all brain work-ups, so the initial diagnosis was given as a primary headache, and symptoms were controlled with painkillers. Medication only worked temporarily, the severe headache persisted, and excessive sweating was seen; also, whenever symptoms occurred, systolic blood pressure increased to more than 180 mmHg.

MRI, MRA and MRV were taken. There were no major abnormalities on MRI and MRA except for a 2 cm sized lipoma (red arrow) on left occipital scalp and focal high signal intensity lesion in periventricular white matter (blue arrow) on FLAIR images (A-C). Hypoplastic veins were seen in left transverse and sigmoid sinuses, but there were no stenosis or occlusions on MRV (D). MRI, magnetic resonance imaging; MRA, magnetic resonance angiography; MRV, magnetic resonance venography; FLAIR, fluid attenuated inversion recovery.
Since the cause of uncontrolled headache was not clear, chest and abdomen computed tomography scans were taken to discriminate hidden malignancies, and an ~4 cm diameter left adrenal gland mass was confirmed (Fig. 2A, B). Subsequently, metanephrine and catecholamine concentrations were measured through 24-hour urine collection, and a dexamethasone suppression test was performed through blood sampling. Urinary metanephrine concentration was 2,236.9 μg/24 hours (normal range: 0–320 μg/24 hours). A metaiodobenzylguanidine (MIBG) scan was performed, and MIBG uptake increased at the left adrenal mass (Fig. 2C). Based on these results, the patient started taking alpha-blocker under the diagnosis of pheochromocytoma, along with controlling blood pressure and headaches, and the pheochromocytoma was removed by surgical treatment. After surgical removal of the mass, he was discharged with no symptoms.
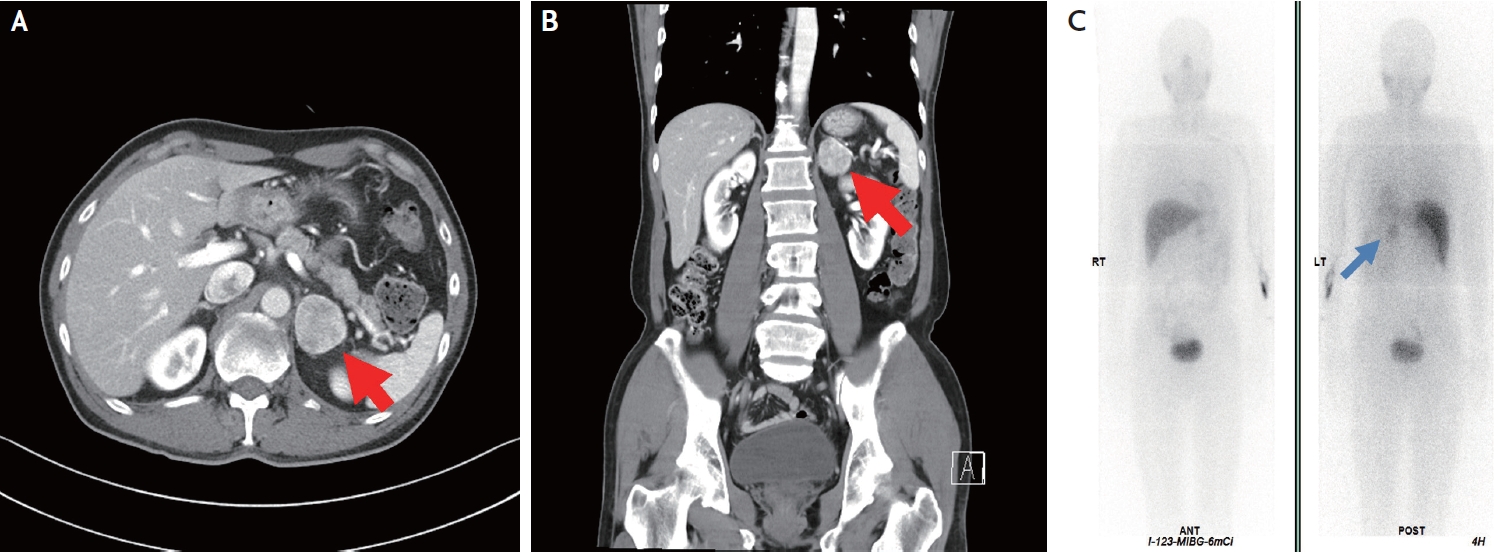
Abdomen CT (A, B) was taken, and an ~4 cm diameter heterogeneously enhanced mass (red arrows) was detected in the left adrenal gland. On the metaiodobenzylguanidine (MIBG) scan (C), MIBG uptake was increased at the left adrenal mass (blue arrow) which suggested pheochromocytoma. CT, computed tomography.
DISCUSSION
Pheochromocytoma is a rare tumor that originates from catecholamine-secreting chromaffin cells derived from the ectodermic neural system and is mostly situated in the adrenal medulla.1 The annual incidence of pheochromocytoma is approximately 0.8 per 100,000 person-years.2 Most doctors will see only one patient with pheochromocytoma in their whole career, and even large hospitals will admit on average only one patient per year.3 A triad of symptoms of paroxysmal headache, excessive sweating, and heart palpitations should raise suspicion of pheochromocytoma, especially when concurrent hypertension exists; however, less than 25% of patients with pheochromocytoma present all three.4 Usually, headaches due to pheochromocytoma occur simultaneously with an abrupt increase in blood pressure. Complications of pheochromocytoma from catecholamine secretion include congestive heart failure, pulmonary edema, myocardial infarction, ventricular fibrillation, cerebrovascular accidents, and catecholamine cardiomyopathy.
In this case, because no abnormalities in whole brain work-ups were found, the headache was treated with medicine as a primary headache; if the pheochromocytoma was not found, it could have caused other serious complications. Because of this, even if all neurological disease is excluded by brain work-up, other causes that can cause severe headaches should not be overlooked.
Notes
Ethics Statement
The requirements for approval of the Institutional Review Board and informed consent were waived due to the retrospective nature of this study.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author upon reasonable request.
Sources of Funding
None.
Conflicts of Interest
No potential conflicts of interest relevant to this article was reported.
Acknowledgements
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science and ICT (NRF-2022R1F1A1074643).
