Unusual Case of Young Age Onset Stroke Suspected to Be Associated with Pseudoxanthoma Elasticum Gene Mutation in ABCC6: A Case Report
Article information
Abstract
Ischemic stroke in young adults can pose diagnostic challenges, particularly when the clinical features deviate from the common presentation. Here, we present the case of a 31-year-old female with transient left-sided hemiparesis. Brain magnetic resonance imaging and angiography revealed right frontoparietal lobe infarction and stenosis of the right internal carotid arteries. Genetic testing revealed a heterozygous variant of unknown significance in the ATP-binding cassette subfamily C member 6 gene NM_001171.6:c.3739C>A (p.Pro1247Thr) that is associated with pseudoxanthoma elasticum, which is a rare disorder characterized by abnormal mineralization of elastic tissues. Although variants of unknown significance can only be classified as causative conditions if all other possible causes are ruled out, this report suggests the importance of considering unusual genetic conditions in young patients with ischemic stroke. Further genetic research, functional studies, and genetic counseling are vital for a comprehensive understanding of these cases.
Ischemic stroke in young adults can present unique diagnostic challenges, especially when the clinical findings are unusual. This case report describes a 31-year-old female who presented with transient hemiparesis. Genetic testing revealed a variant of unknown significance (VUS) in the ATP-binding cassette subfamily C member 6 (ABCC6) gene associated with pseudoxanthoma elasticum (PXE), a rare genetic disorder characterized by abnormal mineralization of elastic tissues.1 This report underscores the significance of considering uncommon genetic disorders in patients with stroke.
CASE
A 31-year-old female with no underlying diseases and no family history of stroke visited our emergency department with transient left-sided hemiparesis of Medical Research Council grade 3. However, the weakness spontaneously resolved within 5 hours of the initial onset, and no neurologic deficit was observed when she arrived at the emergency department. This was the first time that the patient had experienced hemiparesis.
Mild hypertension (159/92 mmHg) was noted in the initial vital signs of the patient. Physical examinations revealed no visible skin lesions. Neurological examination showed no deficits; in particular, the motor grade, sensory changes, cerebellar function, cranial nerve function (such as vision), and ocular eye movement were all unremarkable.
In laboratory tests, low density lipoprotein (112 mg/dL) and homocysteine (23.1 µmol/L) were mildly elevated. Other laboratory test results, including complete blood cell, electrolyte, and chemical tests, were normal. Coagulation and vasculitis related auto-antibody tests, including prothrombin time, d-dimer, anti-thrombin III, Protein C and S, complement, anti-nuclear antibody, anti-neutrophil cytoplasmic antibody, anti-extractable nuclear antigens, lupus anticoagulant, anti-cardiolipin antibody, and anti-β2-glycoprotein were normal.
Imaging was performed 5 hours after initial symptom onset. Brain magnetic resonance imaging revealed diffusion restriction in the right frontoparietal lobes on diffusion-weighted images and a low apparent diffusion coefficient map, confirming acute cerebral ischemic infarction (Fig. 1A, B). Substantial brain atrophy on the right hemisphere was also noted (Fig. 1C, D). Considering the patient’s age, the right-side dominant atrophy implies that cerebrovascular insufficiency may have begun from an early age. Neck computed tomography (CT) angiography showed diffuse segmental decreased caliber of the right internal carotid artery (ICA), with severe stenosis in the right distal ICA and multifocal mild stenosis in the right anterior cerebral artery (Fig. 1E, F). These findings collectively indicated that a genetic abnormality may have caused congenital hypoplasia in the right ICA and subsequently worsened to segmental severe stenosis in the ICA and then finally manifested as hypoperfusion and hypoplasia of the right cerebral hemisphere.
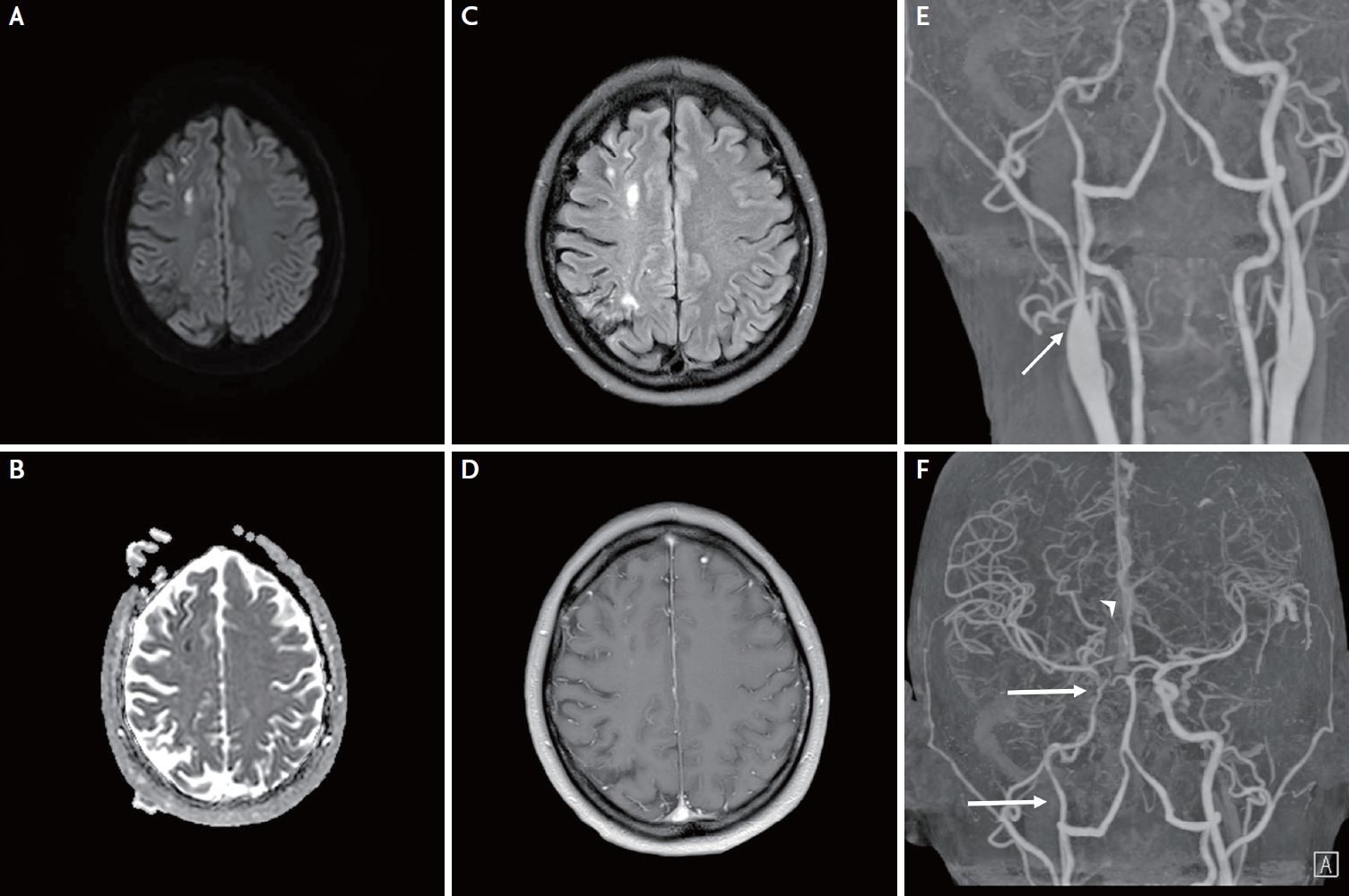
Brain magnetic resonance imaging reveals diffusion restriction in the right frontoparietal lobes in the diffusion-weighted image (A) and low apparent diffusion coefficient map (B), confirming acute cerebral ischemic infarction. High signal intensity is observed in the same lesion on fluid-attenuated inversion recovery imaging (C), while no gadolinium enhancement is noted (D). The right brain hemisphere exhibits substantial brain atrophy compared to the left, considering the patient’s age, implying that cerebrovascular insufficiency may have begun from an early age. Computed tomography angiography shows diffuse segmental decreased caliber of the right internal carotid artery (ICA) with severe stenosis at the distal right ICA (arrow) and multifocal mild stenosis at the right anterior cerebral artery (arrowhead) (E, F).
Given the unusual presentation of a young adult with ischemic stroke, a comprehensive stroke gene panel consisting of 46 known hereditary stroke causative genes was constructed (Supplementary Data 1). Notably, genetic testing revealed a heterozygous VUS in the ABCC6 gene NM_001171.6:c.3739C>A (p.Pro1247Thr). ABCC6 has been associated with PXE, a rare genetic disorder characterized by the mineralization and fragmentation of elastic fibers in various tissues, including the cardiovascular system.
Thorough physical examination to identify cutaneous manifestations, fundoscopy for ophthalmological manifestations, and electrocardiography for arrhythmia were performed, but no abnormalities were found. A young patient with early-onset stroke with a suspected mutation in ABCC6 raised the suspicion that the stroke was caused by PXE. The patient was administered cilostazol and atorvastatin. The patient was discharged without any complications.
DISCUSSION
PXE is an inherited metabolic disorder characterized by the accumulation of minerals and primarily affects elastic tissues such as the skin, eyes, and blood vessels. Prevalence of PXE is approximately 1 in 50,000 individuals, and approximately 150,000 people worldwide have the condition.2 It is caused by mutations in the ABCC6 gene, with an autosomal recessive inheritance pattern.1,3 ABCC6 encodes a protein called the ABCC6 transporter, which is part of a family of transport proteins known as ATP-binding cassette (ABC) transporters.4 The primary function of the ABCC6 protein is to transport molecules that are involved calcium and pyrophosphate (PPi) homeostasis.4,5 Pathogenesis of PXE remains unsolved, but an ABC transporter malfunction may impair PPi removal, a mineralization inhibitor, potentially leading to the accumulation of calcium and other minerals in tissues.5
PXE presents distinct clinical manifestations in the skin, eyes, and blood vessels. Skin involvement includes the development of yellowish bumps or plaques, primarily in areas rich in elastic fibers.1 Ocular symptoms are characterized by the formation of angioid streaks in the retina, potentially leading to vision impairment, while vascular manifestations involve blood vessel calcification, increasing the risk of cardiovascular issues.1-3 Genetic and clinical heterogenicity exist with cardiovascular manifestation, including cerebral aneurysm, arterial dissections, Moyamoya disease, seizures, and strokes.6-9 One recent study showed that PXE may accompany internal carotid artery hypoplasia in patients.10 We also found evidence of congenital hypoplasia of the ICA in this patient on the neck CT angiography. Suspected congenital hypoplasia was further supported by considerable atrophy in the right brain hemisphere, implying that chronic hypoperfusion was present at a very early age, and hypoplasia could be the cause of chronic hypoperfusion and subsequent brain atrophy.
The patient had no atherosclerotic changes and had a relatively well-controlled lipid profile. Comprehensive genetic and laboratory tests for other differential diagnoses, such as vasculitis, Moyamoya disease, and coagulopathy, were negative. The association between the patient’s clinical presentation and VUS in ABCC6 is intriguing; the pathogenicity of the variant NM_001171.6:c.3739C>A (p.Pro1247Thr) has not yet been reported. However, in silico genetic testing (SIFT, PolyPhen, and MutationTaster) predicted that this variant was deleterious; however, this requires further study. Moreover, an interdisciplinary workup on the patient’s disease could not pinpoint any other possible explanations or causative conditions. Therefore, haploid insufficiency of ABCC6 is suspected to lead to dysregulation of calcium and minerals, leading to stenosis of the right ICA. However, functional studies on the targeted genes should be performed in the future to validate the influence of gene mutations.
This case has another interesting point. The patient did not show involvement of skin, eyes, or other blood vessels. Unlike previously reported patients with PXE, who typically exhibit skin lesions and eye involvement, this patient only presented with stroke, and the stroke occurred early in the course of the disease. This could be due to heterozygous haploid insufficiency of the ABCC6 variant, which may not lead to systemic involvement. Further investigations of the patient and additional functional studies are required.
This case underscores the importance of considering rare genetic disorders such as PXE in young adults presenting with ischemic stroke, especially when there are unusual clinical findings. This case also highlights the atypical presentation of PXE; cerebral artery hypoplasia and stroke occurred without any skin lesions or ocular involvement. The presence of a VUS in ABCC6 further complicates the diagnostic process, highlighting the need for ongoing research and genetic counseling. Further investigation of the pathogenicity of the ABCC6 variant is required.
SUPPLEMENTARY MATERIALS
Supplementary materials related to this article can be found online at https://doi.org/10.31728/jnn.2023.00150.
List of comprehensive stroke gene panel consisted of known 46 hereditary stroke causative gene.
Notes
Ethics Statement
This study was approved by the institutional review board at Hanyang University Hospital with a waiver for informed consent (Approval No. HYUH 2023-12-031).
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author upon reasonable request.
Sources of Funding
None.
Conflicts of Interest
No potential conflicts of interest relevant to this article was reported.
Acknowledgements
None.
