Monomelic amyotrophy, also known as focal amyotrophy, is a rare condition that presents with early onset of focal atrophy and weakness, mostly in a single hand and arm. Hirayama disease, one form of monomelic amyotrophy, also known as benign juvenile brachial spinal muscular atrophy, juvenile muscular atrophy of the distal upper extremity, and oblique amyotrophy, progresses over one to five years (less commonly over eight years) and then plateaus.1
Cervical spine magnetic resonance imaging (MRI) in the flexed positions characteristically shows laminodural space widening and anterior displacement of the posterior dura mater in Hirayama disease.2-4
However, in this study, we describe a patient with Hirayama disease who only had prominent isolated spinal cord atrophy without typical MRI findings in the flexed position.
CASE
A 25-year-old man presented to our clinic with insidious onset of progressive right-hand weakness over three months. On physical examination, there was muscle atrophy in right thenar eminence (Fig. 1). The patient had a modified medical research council (MRC) grade of 4 for right fingers extension, while right arm/shoulder muscle power and right fingers flexion/grip power were MRC grade 5. He did not complain of any sensory symptoms. He showed generalized increased reflexes on the deep tendon reflex test on bilateral biceps, triceps, brachioradialis, knee and ankle tendons.
Nerve conduction test and electromyography test showed active denervation potentials in right abductor pollicis brevis and abductor digiti minimi muscles with increased insertional activities in right C8 paraspinal muscles (Fig. 1). Based on his muscle weakness with thenar muscle atrophy and electromyography findings strictly limited on C8-T1 myotome, we suspected monomelic amyotrophy and performed spinal MRI both in the neutral and in the flexed position for trying to identify the characteristic findings of Hirayama disease.
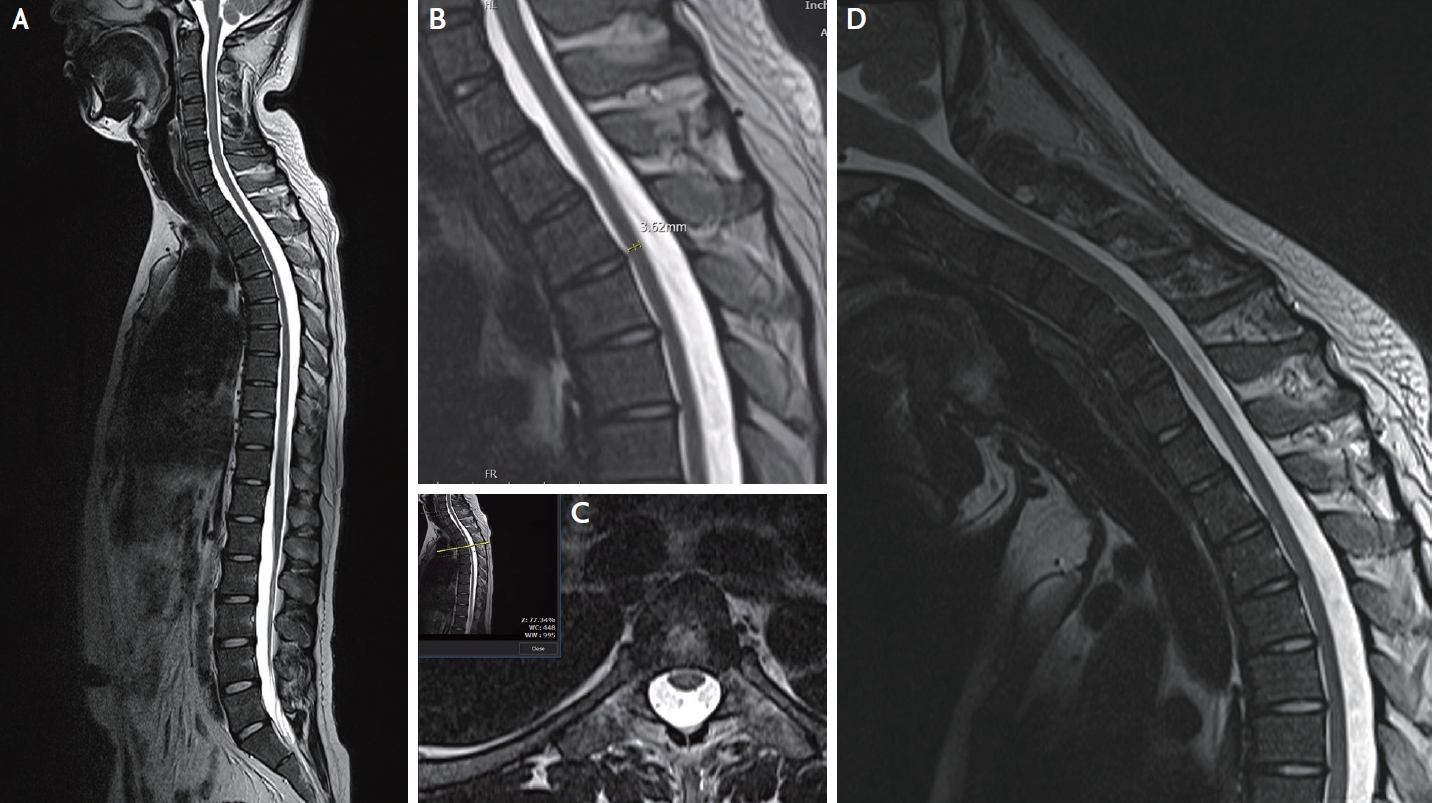
Neutral position sagittal T2-weighted MRI on his spine showed loss of cervical lordosis, and prominent spinal cord atrophy from lower cervical spinal cord down to the upper thoracic cord (Fig. 2A). The anteroposterior diameter of the thoracic cord at T6 levels was approximately 3.6 mm (Fig. 2B).
We performed the spinal MRI to the patient again in the flexed position, but we could not identify the characteristic findings of Hirayama disease, neither anterior displacement of the dura nor a prominent posterior epidural venous plexus compared to the neutral position MR images (Fig. 2D).
Blood tests for Long-chain fatty acid and BSCL2 gene were all negative. During the three-year follow-up period, his symptoms and signs plateaued and did not extend to other myotome segments.
DISCUSSION
In this study, we presented a patient with typical manifestations of Hirayama disease. He had muscle atrophy and weakness strictly confined to the C8/T1 myotome that consistently accorded with electromyographic results. These symptoms and signs plateaued and displayed benign course after a progression period. However, in the MRI evaluation, there was only a prominent isolated spinal cord atrophy without any typical flexion MRI features of Hirayama disease.
Classically, MRI could show an atrophic spinal cord in Hirayama disease, but it has been only with the distinct flexion MRI findings including anterior displacement of the dura and a prominent posterior epidural venous plexus that the diagnosis could become confirmatory.2 But our finding suggests that it may be possible in Hirayama disease to have only spinal cord atrophy without the characteristic flexion MRI findings. When patients exhibit arm weakness and wasting, it’s critical to distinguish Hirayama disease from fatal conditions like amyotrophic lateral sclerosis. From this perspective, it is important to understand both typical and atypical limited findings of the MRI imaging features of Hirayama disease. For supporting our argument, more case reports are needed. There is no established treatment for Hirayama disease. A cervical collar and surgical decompression with fusion have been described in the literature, while most opt for clinical observation.